A bad situation got worse, and it’s time to make serious improvements
By Mike Odeh, Fatima Clark, and Eileen Espejo
July 27, 2022
Top image via iStock from FatCamera
Last month the California Department of Health Care Services (DHCS) released the 2021 Preventive Services Report, which indicates that the COVID-19 public health emergency (PHE) likely had a significant impact on whether children visited health provider locations to receive care, treatment, or screenings. This, of course, is not surprising, but the data underscore the severity with which children’s health services were impacted. For instance, during 2020 child and adolescent well-care visits dropped by 20% and blood lead screenings declined by 17%. The sobering declines during the PHE add to the findings of a 2019 state audit, which found low rates of preventive services for children across California, especially among those in marginalized communities.
Below are the key takeaways from new state and national reports of Medi-Cal (Medicaid) data on children’s health services during the PHE. And while this PHE-related data certainly comes with caveats, these patterns and themes are critical as the State implements the recommendations identified in Medi-Cal’s Strategy to Support Health and Opportunity for Children and Families, released in March.
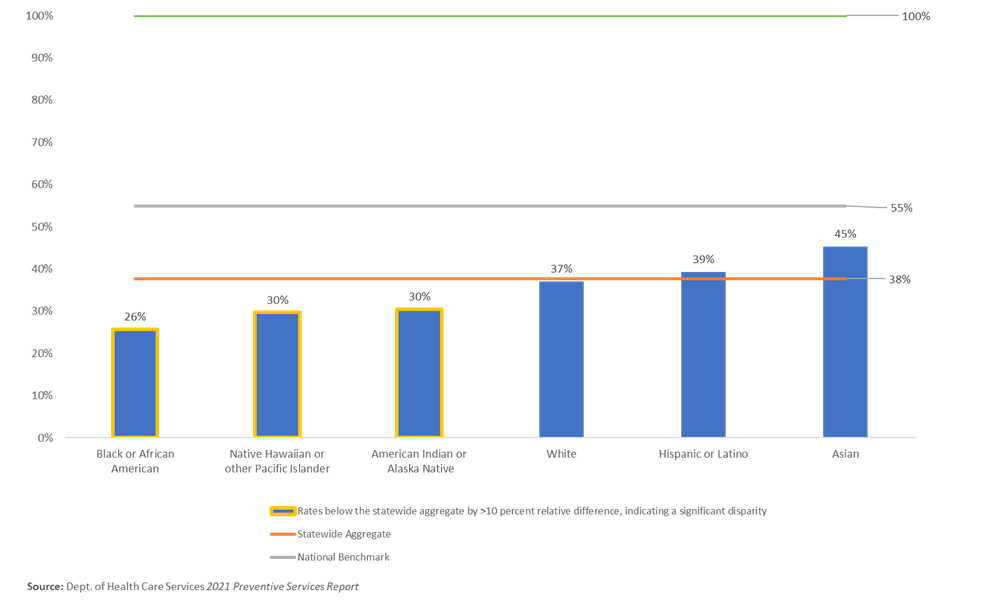
- Persistent disparities in access are harming children of color. Children in communities of color experienced greater declines in health services than other groups, highlighting the disproportionate impact of the PHE on these populations, on top of persistent disparities shown by 2019 data. Specifically in 2020, utilization rates for American Indian or Alaska Native children were significantly below the statewide aggregate for all 19 indicators, and rates for Black children were significantly below the statewide aggregate for 17 of 19 indicators in the Preventive Services Report. Medi-Cal data has consistently shown that Black, American Indian or Alaskan Native, Native Hawaiian, or other Pacific Islander (for example, see graph below), and children living in households that speak a language other than English are not receiving crucial preventive services to which they are entitled. Low quality and utilization rates underscore just some of the health disparities and systemic barriers that underserved communities experience including lack of timely access to health care services; fears about immigration status and public charge; increased transportation challenges; worse environmental conditions, such as poor air quality; and greater racial injustices and cultural biases. Overall deficiencies and inequities in Medi-Cal preventive health care services ultimately puts the health of millions of children of color across the state at risk.
- Children need to catch up on missed services. The federal Centers for Medicare & Medicaid Services (CMS) released a preliminary national Medicaid data snapshot indicating that after major decline in the volume and rate of children’s primary, preventive, and mental health service use during the PHE, rates rebounded through March 2021 for most primary and preventive care services. However, millions of services still need to be delivered to make up for those critical services that were missed between March 2020 and January 2022, especially for routine childhood immunizations. Statewide, the rates of child and adolescent immunizations and infant developmental screenings all declined significantly from 2019 to 2020 according to the latest Medi-Cal Managed Care External Quality Review Technical Report, and it is still not clear if children and youth are caught up on missed vaccines.
- Much more must be done to meet the mental health needs of children and youth. As the Georgetown Center for Children and Families points out, while the number of mental health services provided to adults have nearly returned to pre-pandemic levels, the rate of mental health services for children continues to lag. In fact, the CMS preliminary data show that the rate of mental health services for children generally declined throughout the PHE and had the smallest rebound among all children’s services. Nationally, children’s mental health service use still remains about a quarter (~23%) below pre-PHE levels. During the PHE and a time of unprecedented youth mental health crisis, the California statewide rate for adolescents with a follow-up plan following a positive depression screening was less than 17%. There were also many youth who never even got screened for depression but should have.
- Children’s oral health services also lag behind. In addition to general improvement for physical health services like well-child visits and developmental screenings, there is much room for improvement in children’s oral health care. Preliminary data show the rate of dental services nationally for children remain below pre-PHE levels, with about 18% fewer children receiving services. State data indicate that in 2020, fewer than one in five (19%) young children received dental fluoride varnish from a dental or non-dental provider, despite being an evidence-based preventive service for cavities. Other data published by CMS show that less than half (42%) of kids in Medi-Cal received any preventive oral health service in 2020. To increase dental utilization rates among Medi-Cal kids, DHCS needs to establish and enforce measures to promote and incentivize integration and coordination between medical and dental providers to ensure kids receive all recommended preventive care services.
- States and health plans must be held accountable for delivering care to kids. All of this data should be assisting CMS and DHCS in holding states and Medi-Cal health plans accountable in ensuring children receive adequate and timely access to care. However, the Preventive Services Report shows that rates of children’s services in Medi-Cal are well below the performance benchmarks. For example, across California only 38% of infants completed all pediatrician-recommended well-care visits, far below the benchmark of 55% (see graph below). This discrepancy will be extremely important next year when the State will begin holding plans accountable for meeting minimum performance levels on a set of accountability measures. Due to the PHE, the State has temporarily suspended some enforcement activities and is not holding health plans to meeting those benchmarks based on 2020 data. In acknowledgment of the need for improvement in infant well-child rates, DHCS is participating with seven other states in a CMS Affinity Group on Infant Well Visits, and sharing information and ideas with stakeholders statewide through the Medi-Cal Excellence In Early Childhood Outcomes Collaborative (MEECOC) Learning Community. The ambitious aim of MEECOC is to: “Increase the percent of children in intervention counties who complete two or more well-child visits by 6 months of age by 10 percentage points from the 2021 baseline, and decrease the rate of disparities for at least one racial/ethnic group by 10% from the 2021 baseline.” The MEECOC Learning Community shows a strong commitment to supporting quality improvement and will spur best practices and innovations to deliver better care for kids. Compliance and enforcement are also important tools in holding health plans responsible for providing services to California kids.
California performs well below the national benchmark for infant well care with significant and persistent racial/ethnic disparities among Black, Native Hawaiian or other Pacific Islander, and American Indian and Alaska Native infants in 2020.