By Health Team
June 21, 2023
Top image via iStock from FatCamera
Through the statewide “California Advancing and Innovating Medi-Cal” (CalAIM) initiative, Medi-Cal is seeking to transition from a reactive health care system, in which individuals only receive help when they are sick or hospitalized, to a proactive system of prevention and wellness services. The goal is to reduce health inequities and achieve better health outcomes for the highest need beneficiaries in Medi-Cal by integrating services, facilitating community resources, addressing social determinants of health, and decreasing inappropriate utilization and duplication of services. Especially for California’s most vulnerable children, a stronger emphasis on prevention and addressing unmet social needs can change a child’s entire health trajectory.
With the launch of the CalAIM initiative, the Department of Health Care Services (DHCS) has designed a Population Health Management program to ensure that Medi-Cal enrollees have access to a comprehensive set of health care and social services based on their individual or family needs and preferences. As part of that, DHCS has also designed a new approach, Enhanced Care Management (ECM), to better support Medi-Cal children and youth with complex clinical and non-clinical needs who access care in multiple delivery systems.
Here is what you need to know:
What is Enhanced Care Management (ECM)?
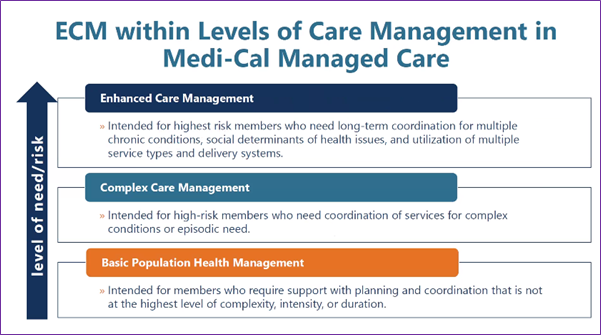
In order to understand ECM it is important to understand that all children require some basic level of care management, which includes preventive care and check-ups, age-specific screenings and assessments, coordination of care between specialties and providers, access to oral health services, and help accessing social, educational, and developmental services in addition to physical care. Some children, however, need a bit more support and coordination of services, for example, if they have a chronic condition or are recovering from an accident or illness; this is called “Complex Care Management.”
There are still other kids who are experiencing significant health and social needs who may benefit from ongoing and intensive support across services and systems. These could include youth who are high utilizers of the emergency department, at high-risk of life-threatening mental health crises, or whose needs are beyond what the California Children’s Services (CCS) program already provides for children and youth with special health care needs. (See visual below and box on care management definitions.)
So, starting July 1, 2023, Managed Care Plans (MCPs) will begin offering additional, intensive care level of supports to some children and youth. This new voluntary benefit is called “Enhanced Care Management,” and will provide children with a single Lead Care Manager who will coordinate care and services among the physical, behavioral, dental, developmental, and social services delivery systems, making it easier for kids to get the right care at the right time. ECM aims to provide a whole-person approach to care that addresses the circumstances of high-need members enrolled in Medi-Cal managed care.
To provide ECM services, plans will contract with a network of ECM providers that may include, but are not limited to: CCS providers, school-based health centers, primary care physicians, community health centers, local health departments, Indian Health Service Programs, First 5 County Commissions, community based organizations, and behavioral health entities.
Care Management Levels in Medi-Cal Managed Care
- Basic Population Health Management (BPHM) is an approach to care that ensures that needed programs and services are made available to each member, regardless of their risk tier, at the right time and in the right setting. BPHM includes federal requirements for care coordination (as defined in 42 C.F.R. § 438.208).
- Complex Care Management (CCM) is an approach to care management that meets differing needs of high-and rising-risk members, including both longer-term chronic care coordination and interventions for episodic, temporary needs. Medi-Cal Managed Care Plans (MCPs) must provide CCM in accordance with all National Committee for Quality Assurance (NCQA) CCM requirements.
- Enhanced Care Management (ECM) is a whole-person, interdisciplinary approach to care that addresses the clinical and nonclinical needs of high-cost and/or high-need members who meet ECM Populations of Focus eligibility criteria through systematic coordination of services and comprehensive care management that is community-based, interdisciplinary, high-touch, and person-centered.
Source: DHCS’ Population Health Management Policy Guide
Who is eligible for ECM?
Some populations of Medi-Cal enrollees – mostly adults – are already eligible for ECM services. As of September 2022, over 88,000 Medi-Cal members were receiving ECM services since the new benefit launched on January 1, 2022. The state has identified eight groups of children and youth that will be eligible for ECM services starting on July 1, 2023. These groups of children and youth (or “Populations of Focus”) include:
- Homeless families or unaccompanied children/youth experiencing homelessness
- Children and youth at risk for avoidable hospital or emergency department utilization
- Children and youth with serious mental health and/or substance use disorder needs
- Children and youth transitioning from a youth correctional facility
- Children and youth enrolled in CCS or CCS Whole Child Model with additional needs beyond the CCS condition
- Children and youth involved in child welfare
- Children and youth with intellectual or developmental disabilities
- Pregnant or postpartum youth
Source: DHCS’ Enhanced Care Management Policy Guide
For children already enrolled in programs like CCS, the ECM benefit will enhance and seamlessly integrate with existing care management services in those programs, and plans must ensure non-duplication of services between ECM services and services provided by other programs.
How can you find out more about ECM?
The ECM benefit is administered by the plans, so the best way to find out what ECM services for children and youth are available in your area is to contact your Managed Care Plan.
To request care coordination support, transportation, language assistance, or access to a Community Health Worker, contact your child’s plan.
How will ECM change the care coordination landscape for families?
To try to answer this question, Children Now commissioned a series of focus groups among parents of children in the California Children’s Services (CCS) program held in May 2023. Overall, there was a general lack of awareness about the ECM benefit among parents, and guarded optimism about how well it might work and how it might change their child’s health care experience.
- What does care coordination look like today? In the current system, families must often work tirelessly to coordinate their child’s care and manage the calendar of appointments. However, there is a reported lack of communication between parents and providers and caseworkers, and the burden is often on parents to seek out available services and find transportation. Some children have needs that are too complex for a single care coordinator. Caseworkers often have high caseloads and may not have timely or necessary knowledge about information on services. Also, not all care that children need is sufficiently accessible, such as dental services and therapies for autism spectrum disorders.
- What are the hopes for and concerns about ECM? When asked about how ECM may change their experiences, parents expressed concerns about losing their child’s current provider(s) and/or case managers, with whom there is established trust and knowledge about their child’s needs. Parents also expressed wanting their communications needs met in more languages, specifically in Spanish and Cantonese, and through multiple information channels, such as email, text message, social media, resource webpage(s) specifically for ECM, and through peers and community groups (one suggestion was training of parent “ambassadors” for ECM). As part of better coordination, parents also expressed the desire for more accommodating spaces for siblings of children receiving care or therapies, e.g. a waiting room with games.
Support for this research was provided by the Lucile Packard Foundation for Children’s Health. The views presented here are those of the authors and not necessarily those of the Foundation or its directors, officers or staff.


